
What Is GERD and Why Do Runners Experience It?
GERD (Gastroesophageal Reflux Disease) is a condition in which stomach acid flows back into the esophagus, causing symptoms such as heartburn, chest discomfort, nausea, shortness of breath, and sleep disturbance. It is often treated as a purely gastrointestinal issue, but GERD is surprisingly common among runners and endurance athletes.
In runners, symptoms can be aggravated by:
- Repetitive vertical impact and changes in intra-abdominal pressure
- Running soon after meals
- Sleeping soon after meals
- Inefficient breathing patterns
- Chronic stress and autonomic nervous system imbalance
While medications and dietary changes are often helpful, they do not always address why the body is predisposed to reflux in the first place.
Why Physical Therapy Can Help GERD
GERD is not only a stomach problem. It is closely related to:
- Diaphragm function and breathing mechanics
- Autonomic nervous system regulation (sympathetic vs. parasympathetic)
- Visceral mobility of the stomach and esophagus
- Postural and cervical–thoracic tension
Physical factors that may affect the GERD symptoms

Diaphragmatic function
Nervous system
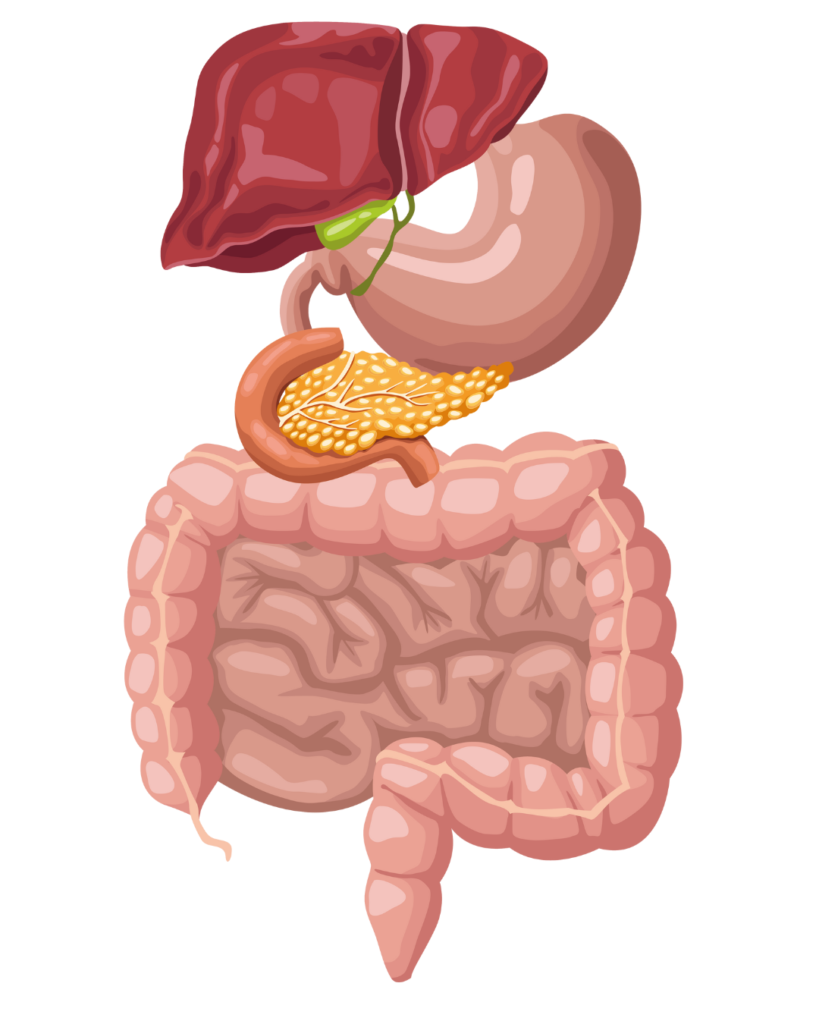
Organ mobility

Posture
From a physical therapy perspective, addressing these systems together can significantly reduce symptoms and improve overall function—especially in runners.
Case Study: A Runner With GERD Symptoms
Initial Presentation
This patient was a recreational runner experiencing persistent GERD symptoms that interfered with both daily life and training. Her main complaints included:
- Inability to sleep flat due to uncomfortable reflux sensations
- Shallow breathing, difficulty swallowing (dysphagia) with constant tension in the neck, chest, and upper trunk
- Nausea during running, especially after eating
Running felt increasingly uncomfortable, and her symptoms negatively affected her performance and recovery. The patient described symptoms as extremely frustrating, noting that her legs felt fine, yet reflux symptoms prevented her from running.
A comprehensive assessment revealed:
- Inefficient diaphragmatic movement
- Signs of decreased soft tissue mobility around vagus (parasympathetic) nerve
- Excessive tone in the cervical spine, cranial region, and upper thorax
Overall, her presentation suggested a hyperactive sympathetic nervous system, keeping her body in a constant “fight or flight” state.
Treatment Approach 1: Visceral Manipulation
Treatment began with visceral manipulation targeting the stomach and surrounding tissues. The goal was to restore normal mobility and glide of the abdominal organs, particularly their relationship with the diaphragm.
Improving visceral mobility helped:
- Reduce mechanical stress at the gastroesophageal junction
- Improve coordination between breathing and abdominal pressure
Treatment Approach 2: Vagus Nerve–Focused Intervention
Because parasympathetic regulation plays a key role in digestion, treatment also focused on supporting vagus nerve function.
Gentle manual therapy techniques were applied to the cervical and cranial regions to:
- Promote parasympathetic activation
- Reduce excessive sympathetic tone
- Improve overall autonomic balance
Treatment Approach 3: Diaphragmatic Breathing Re-education
The patient was instructed in diaphragmatic breathing to improve breathing efficiency and pressure management.
This intervention aimed to:
- Normalize intra-abdominal pressure during rest and running
- Support the anti-reflux function of the diaphragm
- Reduce upper chest and neck overactivation
- Facilitate parasympathetic nervous system activity
Treatment Approach 4: Cervical, Cranial, and Upper Thoracic Manual Therapy
Due to chronic stress and protective guarding, the patient demonstrated significant tension in the upper trunk.
Manual therapy was provided to the cervical spine, cranial structures, and upper thorax to:
- Decrease muscular and neural tension
- Create a physical environment that allows the nervous system to downregulate
Outcomes
After several sessions:
- The patient was able to sleep comfortably on a flat surface
- Breathing felt deeper and more relaxed
- Nausea during running significantly decreased
- Running felt smoother, with noticeable improvement in performance and comfort
These changes highlighted the importance of addressing the nervous system, breathing mechanics, and visceral mobility together, rather than treating GERD as an isolated digestive issue.
Physical Therapy as a Holistic Option for Runners With GERD
Medical management or dietary guidance may still be necessary for GERD. However, it can be a powerful complementary approach by addressing the underlying physical and neurological contributors to reflux.
For runners who experience GERD symptoms during training or sleep, evaluating breathing patterns, autonomic balance, posture, and visceral mobility may reveal missing pieces of the puzzle.
GERD does not have to limit running performance. With a holistic, individualized approach, physical therapy can help runners breathe better, sleep better, and run with greater comfort and confidence.


