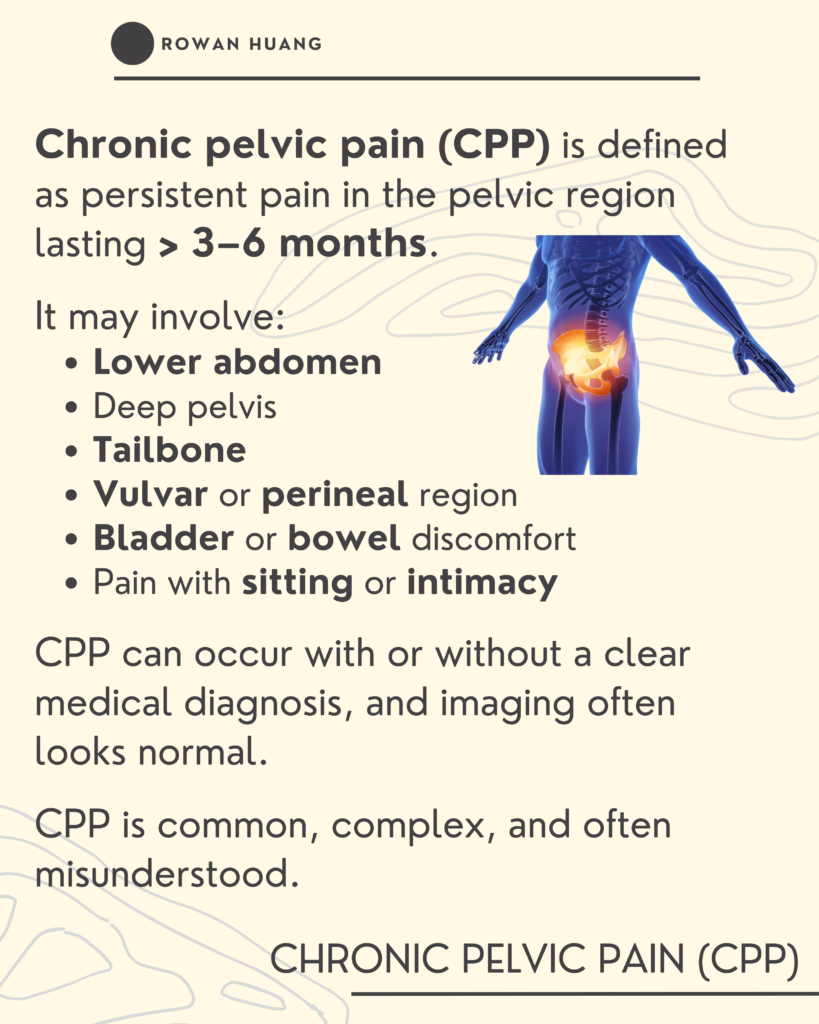
Chronic Pelvic Pain (CPP) is defined as persistent pain in the pelvic region lasting longer than 3–6 months.
It may involve:
- Lower abdominal pain
- Deep pelvic pain
- Tailbone discomfort
- Vulvar or perineal pain
- Bladder or bowel irritation
- Pain with sitting or intimacy
Imaging often looks normal, but the pain is very real.
CPP is common, complex, and often misunderstood.
It’s rarely just a joint issue.
In the early stages, pain may begin as tissue-based (nociceptive pain).
As I discussed in my previous post on pain mechanisms, pain does not always remain tissue-driven.
When pain persists, the nervous system can become more protective.
This is where nociplastic mechanisms may begin to play a role.
The system becomes more sensitive, even if tissue healing has already occurred.
Why is the pelvic region particularly vulnerable?
Because the pelvis is:
- A major load transfer zone
- Closely connected to stress and emotional processing
- A common site of postpartum and persistent pain
- A complex intersection of musculoskeletal, visceral, hormonal, and neural systems
The pelvic floor plays a significant role.
It is part of your deep core system, working together with:
- The diaphragm
- The transverse abdominis
- The deep spinal stabilizers
In chronic pelvic pain, the pelvic floor is often not weak.
More commonly, it may be:
- Overactive
- Guarded
- Lacking coordination
- Unable to fully relax
When the nervous system stays in protection mode,
the pelvic floor may remain tense even when it doesn’t need to.
Over time, this sustained guarding can reinforce the pain cycle.
Chronic pelvic pain is often a systems issue.
Not just structure.
Not just strength.
Not just alignment.
It may involve:
- Load transfer strategies
- Breathing mechanics
- Pelvic floor coordination
- Stress physiology
- Nervous system sensitization
Many people with persistent pelvic pain are not unstable.
They’re overprotective.
Pelvic health physical therapy is more than just Kegels, internal work, or “fixing alignment.”
It may involve:
✓ Teaching relaxation before strengthening
✓ Improving coordination before force
✓ Gradual exposure to load
✓ Rebuilding safety in movement
✓ Pain education
Recovery isn’t about locking the pelvis down.
It’s about restoring adaptability.
Want to learn more or book a session?
Book your visit here and start your recovery journey!