Many people assume pain always means tissue damage.
But clinically, pain is more complex than that.
Understanding the mechanism behind pain often explains why symptoms behave the way they do — and why some treatments work while others don’t.
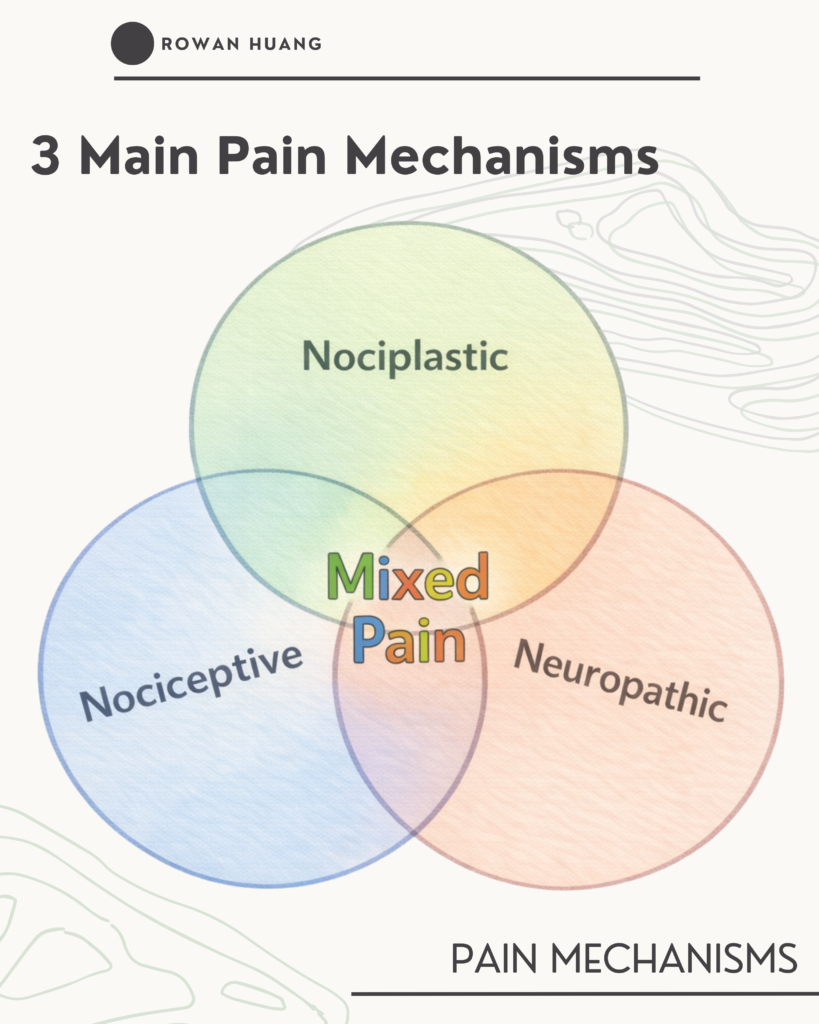
There are three main pain mechanisms.
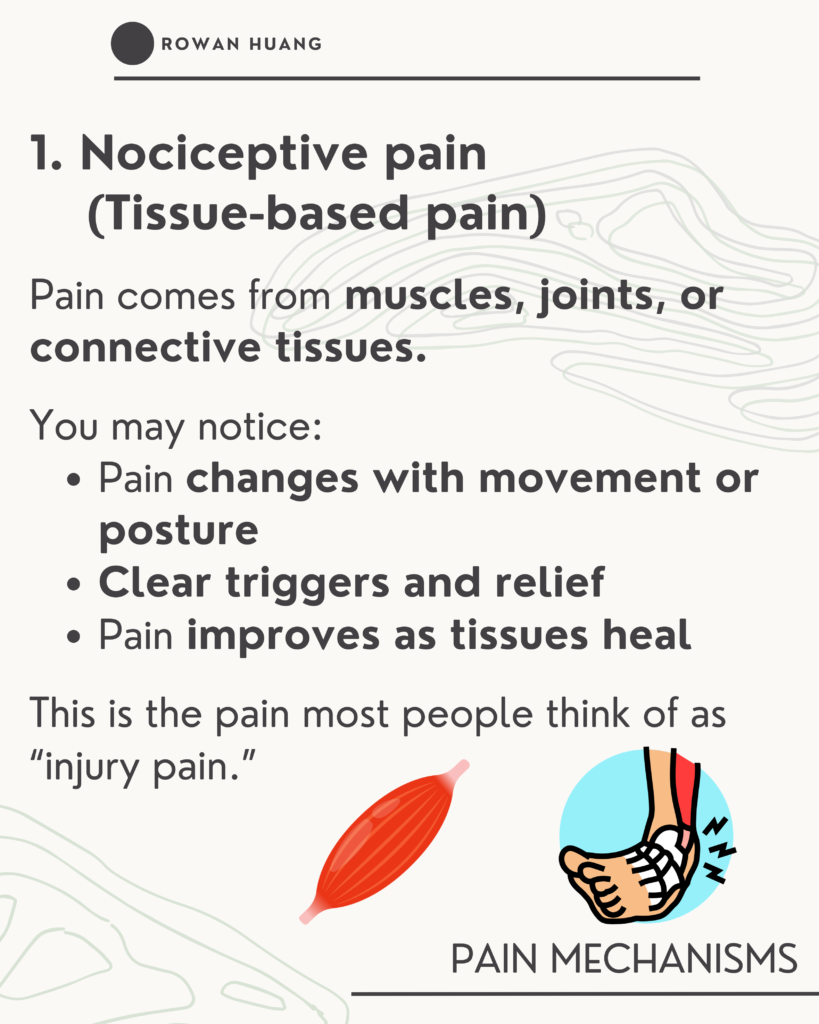
1. Nociceptive Pain (Tissue-Based Pain)
This type of pain comes from muscles, joints, ligaments, or connective tissues.
Common features:
- Pain changes with movement or posture
- Clear aggravating and easing factors
- Symptoms improve as tissues heal
This is typical “injury pain.”
When load is managed appropriately, recovery usually follows.
2. Neuropathic Pain (Nerve-Related Pain)
This occurs when the nervous system itself is affected, such as with nerve irritation or compression.
Common features:
- Burning, electric, or shooting sensations
- Tingling or numbness
- Symptoms following a nerve distribution
This type of pain is not simply muscle tightness or inflammation.
It requires a different treatment focus.
3. Nociplastic Pain (Sensitized Nervous System)
In this case, pain is real, but there is no clear tissue or nerve damage explaining the intensity.
The nervous system remains in a protective state.
Common features:
- Widespread or unpredictable symptoms
- Pain out of proportion to activity
- Persistent pain beyond expected tissue healing
- Flare-ups with stress, poor sleep, or fatigue
Here, the system has become overly sensitive.
A Key Clinical Reality
Pain is rarely just one mechanism.
Most persistent pain presentations are mixed
(for example, tissue irritation combined with nervous system sensitization).
Importantly, the dominant driver can change over time.
Why Identifying the Mechanism Matters
Different mechanisms require different treatment priorities:
- Tissue-dominant pain → Load management and movement rehabilitation
- Nerve-dominant pain → Reducing irritation or compression of the nerve
- Sensitization-dominant pain → Calming the nervous system and gradually rebuilding tolerance
If every presentation is treated as “just tight muscles,” progress often stalls.
Clinical reasoning focuses on identifying the predominant mechanism at a given point in time to guide treatment direction.
What Research Tells Us
There is no single test that can definitively identify pain mechanisms.
- MRI scans do not show pain
- X-rays do not explain symptoms
- No single questionnaire provides the full answer
Pain must be understood by integrating:
- Your symptom history
- Behavior of symptoms over time
- Movement and sensory responses
- Clinical examination findings
No single result tells the whole story.v
Final Takeaway
Pain is real.
But pain is complex.
Not all pain is driven by the same mechanism and effective treatment should reflect that complexity.
Understanding what is driving your pain is often the first step toward meaningful improvement.
If you’re dealing with persistent or chronic pain, book a 1-on-1 assessment via the link below.
https://docs.google.com/forms/d/e/1FAIpQLScZFwLgKq3fSEROF3iT38pa12RG9A-hAgK7OX_HkdqQjnpMrw/viewform